Thinking about dental implants but not sure what the process actually involves? You’re not alone. Dental implants can seem complicated until you break the procedure down step by step. This article explains how each stage of the process works, from your first consultation to final recovery, so you can feel confident about moving forward. It’s not just about replacing teeth. It’s about restoring your health, comfort, and quality of life.
Dr. Bethaney B. Brenner DMD and her caring team offer expert implant care designed around comfort, clarity, and long-term results. With over 40 years of experience in dentistry and advanced surgical training, Dr. Brenner provides personalized solutions for patients across Burlington, including those in Whigville, Angela’s Way, and the Farmington River Valley. Her patient-first approach and holistic treatment planning make her one of the most trusted implant dentists in the region.
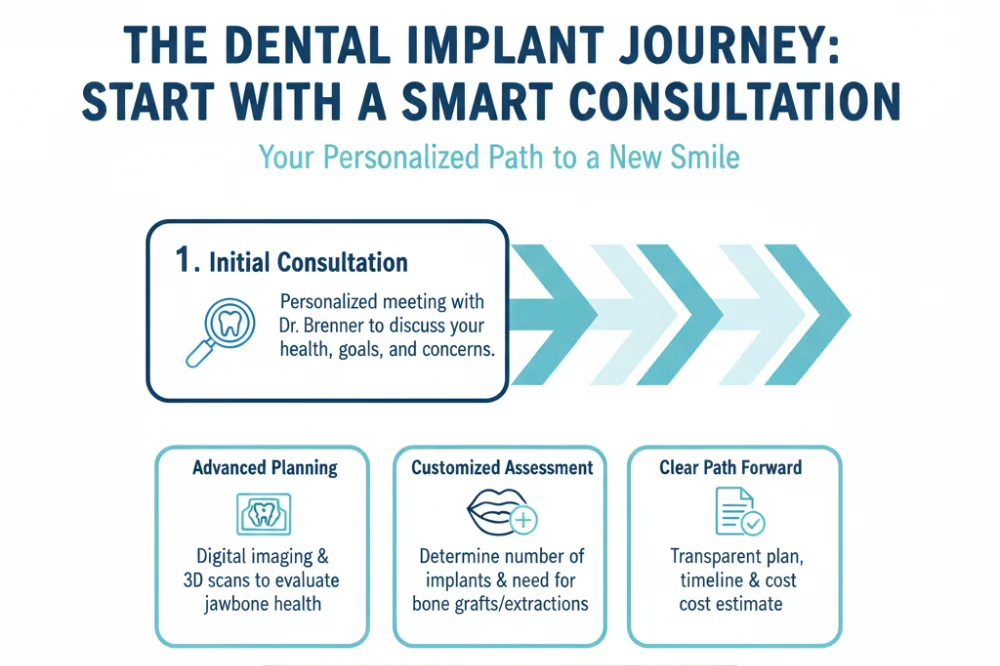
How the Dental Implant Process Begins
Every implant journey starts with a personalized consultation. Dr. Brenner takes time to understand your goals, review your health history, and examine your oral structure using 3D scans and digital imaging. She’ll assess the number of teeth to replace and determine whether your jawbone is strong enough for implants. If needed, she’ll also outline any preparatory steps like bone grafting or extractions.
Patients from Bittersweet Lane, East Burlington, and West Burlington often say this appointment helped them feel more confident about what was ahead. There’s no sales pitch, just expert insight tailored to your situation and questions.
Comparing Implant Treatment to Other Tooth Replacement Options
When you’re deciding how to replace missing teeth, it’s important to look beyond the short-term fix. Dental implants often feel like a bigger commitment up front, but their advantages extend far beyond initial placement. Patients frequently ask how implants stack up against other options like bridges or dentures, not just in terms of cost, but also comfort, function, and longevity. Understanding these differences can help you make a decision that supports your health for years to come.
| Feature | Dental Implants | Traditional Bridge | Full Denture |
| Longevity | 20+ years with proper care | 5–15 years | 5–10 years |
| Affects Nearby Teeth | No | Yes (adjacent teeth altered) | No |
| Bone Preservation | Yes | No | No |
| Comfort & Stability | Very high | Moderate | Can slip or shift |
| Upkeep Costs Over Time | Low | Medium | Medium to high |
Implants stand out because they actively preserve jawbone health while restoring natural bite strength and stability. Unlike bridges, they don’t rely on neighboring teeth for support. And unlike dentures, they won’t move around or create pressure points during daily use. That kind of durability and comfort is why so many patients from Collinsville, Jerome Avenue, and Alpine Drive see implants as a smart long-term investment, even if the upfront cost is slightly higher.
Surgical Placement of the Implant Post
Once the treatment plan is set, the next step is placing the titanium implant post. This is the anchor for your future tooth. The procedure is done under local anesthesia, and IV sedation is available if requested. Dr. Brenner uses surgical guides and precise digital imaging to place the implant safely and accurately.
Most patients report minimal discomfort after surgery, comparing it to a simple extraction. Healing begins right away, and over the next few months, the bone fuses with the implant in a process called osseointegration. This stage is essential for creating a strong, lasting foundation.
Key Benefits You Can Expect Along the Way
Throughout the implant journey, patients report a variety of functional and emotional benefits. These improvements often show up gradually, but they make a lasting difference in everyday life.
- Stronger bite function: Implants restore full chewing ability, allowing patients to enjoy a wider variety of foods without discomfort.
- Improved speech: Missing teeth or ill-fitting dentures can alter speech. Implants provide stability that helps restore natural pronunciation.
- Preserved bone structure: Unlike dentures or bridges, implants stimulate bone and prevent facial collapse.
- No impact on nearby teeth: Implants stand on their own, so surrounding teeth don’t need to be filed down like they would with bridges.
- Increased confidence: From professional settings to social situations, many patients report smiling more and feeling more at ease.
These benefits aren’t just cosmetic, they’re foundational to long-term wellness and quality of life. That’s why patients across Spielman Highway, Stanwich Lane, and Angela’s Way often call implants the best decision they’ve made for their health.
Abutment Placement and Custom Crown
After the bone has fully healed, the next phase begins. Dr. Brenner places a small connector called an abutment on top of the implant post. This piece will support the final crown or bridge. In some cases, the abutment is placed during the initial surgery, but it’s often done separately after healing is complete.
From there, Dr. Brenner captures a digital scan or impression to design your final restoration. She partners with expert labs to ensure that each tooth looks natural and feels completely comfortable. The final crown is crafted to match your existing teeth in both color and shape, and it’s permanently secured to the abutment.
Patients often describe this final visit as the most exciting part of the process. After months of preparation, you get to enjoy a complete, natural-looking smile that blends seamlessly with the rest of your teeth.
What to Expect at Your Consultation
The consultation is more than just an exam. It’s a hands-on planning session where you and Dr. Brenner decide on your path forward. She’ll explain the sequence of treatment, highlight any special considerations, and walk you through options tailored to your timeline, comfort level, and budget.
By the end of the visit, you’ll leave with:
- A clear understanding of whether implants are the right choice for you
- A proposed timeline that includes healing and placement stages
- Transparent pricing and information about available financing options
- A realistic plan for any preliminary procedures like bone grafts or extractions
Patients from Riverview, Savarese Lane, and Lost Acres appreciate the time taken to answer questions honestly and thoroughly. There’s no pressure, just partnership and clarity from day one.
Taking the Next Step Toward a Stronger Smile
Dental implants aren’t just a procedure, they’re a pathway back to full function and self-confidence. At every step, Dr. Bethaney B. Brenner DMD brings unmatched experience, advanced surgical skill, and a commitment to patient-first care. Her credentials, training, and years of service in the Connecticut State Dental Association speak to her credibility and compassion.
If you’re ready to take the next step toward a lasting, comfortable solution for missing teeth, we’re here to help. Call our Burlington office today to schedule your consultation and start your journey with a team that always puts your health and comfort first.
Book Your Consultation Today!
Dr. Bethaney B. Brenner DMD
8 Milford St, Burlington, CT 06013
(860) 673-7155
Frequently Asked Questions
How long does the dental implant process take?
Patients want to know how long they’ll be “in treatment,” from first consult to final tooth.
What they should ask instead: What’s a realistic timeline from implant placement to final crown, and what can lengthen or shorten that process?
- Immediate Insight: For a straightforward case, the full dental implant process commonly takes about 3–9 months from planning to final crown. This includes time for the implant to fuse with the jawbone (osseointegration), which is what makes implants so stable.
- Supporting Context: Typical stages include consultation and planning, implant surgery, a 3–6 month healing/osseointegration period, then placement of the abutment and custom crown; some patients qualify for faster or same‑day approaches, while others need extra time if extractions or bone grafts are involved.
- Deeper Implication: Your individual timeline depends on bone quality, whether grafting or sinus lift is needed, how you heal, and whether your dentist uses traditional or immediate‑load protocols, your treatment plan should spell this out clearly at the start.
Will I be in pain after implant surgery?
Fear of pain is one of the biggest reasons people delay implants.
What they should ask instead: What does normal post‑implant discomfort feel like, and how is it usually managed?
- Immediate Insight: Most patients describe post‑implant discomfort as mild to moderate, similar to or a bit easier than a tooth extraction. Soreness, swelling, and tenderness around the site for a few days are common and typically controlled with over‑the‑counter pain relievers your dentist recommends.
- Supporting Context: Professional guidance from dental organizations notes that local anesthesia is used during surgery, and many people return to normal daily activities within a day or two, though chewing on the surgical side and heavy exercise are often limited briefly.
- Deeper Implication: Following the written aftercare (ice, soft foods, prescribed or OTC medications, and good oral hygiene) is what keeps discomfort short‑lived; severe or worsening pain is a cue to call the office promptly for evaluation.
Is everyone a candidate for dental implants?
Patients want to know if health conditions or bone loss automatically rule them out.
What they should ask instead: What health and bone conditions do I need for a safe, successful implant?
- Immediate Insight: Many healthy adults are candidates for implants, but you must have enough jawbone and healthy gums to support them, and be able to heal normally. Conditions like uncontrolled diabetes, heavy smoking, or certain medications can affect healing and success rates.
- Supporting Context: Oral and maxillofacial surgery guidelines explain that a clinical exam plus imaging (often 3D scans) are used to assess bone volume, nerve locations, and sinus anatomy; these findings guide whether standard implants, grafting, or alternative options are best.
- Deeper Implication: Being told you’re “not a candidate yet” often means you may benefit from preparatory treatment, such as bone grafting, periodontal care, or smoking reduction, rather than being permanently excluded from implants.
What if I need a bone graft before my implant?
Hearing “you need a bone graft” can sound intimidating and patients want to understand why it’s recommended.
What they should ask instead: How does a bone graft change my timeline, and what benefits does it provide for my implant?
- Immediate Insight: A bone graft is used when the jaw is too thin or soft to hold an implant securely. It rebuilds or thickens the area so the implant has a strong, stable foundation, which significantly improves long‑term success.
- Supporting Context: Depending on the size and type of graft, healing often takes several months, commonly about 3–6 months, and in some large or sinus‑lift cases up to 6–9 months, before the implant can be safely placed.
- Deeper Implication: While a graft adds time up front, it reduces the risk of implant loosening or failure later, making it a key investment in durability rather than a setback; your dentist or surgeon should explain graft type, healing expectations, and how it fits into your overall schedule.